20 AMERICAN HABITS
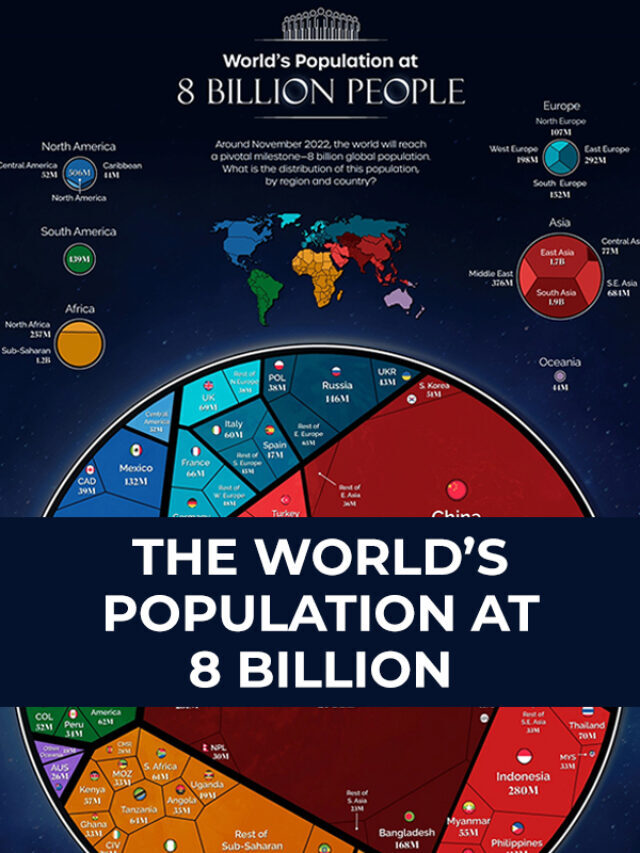
The World’s Population at 8 Billion
PREMIER LEAGUE 2022 – 23 / ALL YOU NEED TO KNOW
The best mechanical keyboards to buy right now
Miss Texas R’Bonney Gabriel as First Filipino-American to Win Miss USA
Scientists Have Discovered a New Set of Blood Groups
The ‘Er’ grouping could help doctors identify and treat some rare cases of blood incompatibility, including between pregnant mothers and fetuses.

The unborn baby was in trouble. Its mother’s doctors, at a UK hospital, knew there was something wrong with the fetus’s blood, so they decided to perform an emergency C-section many weeks before the baby was due. But despite this, and subsequent blood transfusions, the baby suffered a brain hemorrhage with devastating consequences. It sadly passed away.
It wasn’t clear why the bleeding had happened. But there was a clue in the mother’s blood, where doctors had noticed some strange antibodies. Some time later, as the medics tried to find out more about them, a sample of the mother’s blood arrived at a lab in Bristol run by researchers who study blood groups.
They made a startling discovery: The woman’s blood was of an ultrarare type, which may have made her baby’s blood incompatible with her own. It’s possible that this prompted her immune system to produce antibodies against her baby’s blood—antibodies that then crossed the placenta and harmed her child, ultimately leading to its loss. It may seem implausible that such a thing could happen, but many decades ago, before doctors had a better understanding of blood groups,
Through studying the mother’s blood sample, along with a number of others, scientists were able to unpick exactly what made her blood different, and in the process confirmed a new set of blood grouping—the “Er” system, the 44th to be described.
You’re probably familiar with the four main blood types—A, B, O, and AB. But this isn’t the only blood classification system. There are many ways of grouping red blood cells based on differences in the sugars or proteins that coat their surface, known as antigens. The grouping systems run concurrently, so your blood can be classified in each—it might, for instance, be type O in the ABO system, positive (rather than negative) under the Rhesus system, and so on.
Thanks to differences in antigens, if someone receives incompatible blood from a donor, for example, the recipient’s immune system may detect those antigens as foreign and react against them. This can be highly dangerous, and is why donated blood needs to be a suitable match if someone is having a transfusion.